Your child’s been
diagnosed with NF1
(Neurofibromatosis Type 1)



Your child’s been
diagnosed with NF1
(Neurofibromatosis Type 1)
NF1



What is NF1?
General symptoms of NF1
Café-au-lait Spots: Light brown skin spots that look like birthmarks.
Freckling: Freckles in unusual places, such as the armpits or groin.
Lisch Nodules: Tiny bumps on the iris of the eye, which usually don’t affect vision.
Neurofibromas: Soft, benign (non-cancerous) tumours that can develop on or under the skin.
Learning Disabilities: Some children with NF1 may have learning challenges or ADHD.
Bone Abnormalities: Some may have issues like scoliosis (curved spine) or bowed legs.
Diagnostic criteria for NF1
Six or more café-au-lait spots*
Tumours
Freckling
Two or more Lisch nodules
Lisch nodules are yellow brown dots on the iris of the eye.
Or two or more abnormalities in the choroid
The layer of the eye containing blood vessels.
Optic glioma
Bone abnormalities
A first-degree relative with NF1
Understanding the difference
Symptoms
Diagnostic criteria
Understanding the pathway of the NF1 gene
Understanding the pathway of the NF1 gene
A parent with NF1 based on diagnostic criteria
Genetic tests are not always required, but they may be suggested when there is no clear diagnosis, possibly because visible symptoms are not obvious or have yet to develop.
Genetic testing for NF1 is a valuable tool but it is not infallible. While highly accurate there is a small risk of a false negative in 2 – 5 % of cases, meaning that the mutation in the NF gene may not be detected even if it is present. Because of this, genetic testing is used to support, rather than replace clinical diagnostic criteria
This means that there must be at least one other diagnostic feature present to confirm NF1.
What should I tell my child about their diagnosis?
Be honest with your child from the start and be open about the condition with them and those around them. Childhood Tumour Trust have a booklet you can read online, featuring their mascot ‘Patches’, to help explain to children their diagnosis – you can order a printed copy here. There is also a video to watch for other people such as family and friends.
What happens after Diagnosis?
Now that your child has been diagnosed, you may be wondering what happens next. You can read online or order a booklet based on this website to help manage your child’s care. You can download our insert for the Red RCPCH Child Development Book – or use it on its own if your child doesn’t have one. It helps you and your healthcare provider track key health concerns, along with the NF1 Review Checklist for children and adults. Your child might not be prescribed any treatment in the first instance. Instead, you may be asked to keep a close eye on your child’s health and behaviour, to monitor for any changes. Such changes can include:
-
New lumps or bumps, or changes to existing ones
-
Headaches
-
Alterations to speech
-
Changes in their ability to move around
-
Difficulties with social interactions
-
Sensitivity to light, noise, touch, tastes, or smells
-
Changes in eyesight
Quite often families of children with NF1 will hear the phrase, ‘watch and wait’ or something similar. What this means and how to deal with this period of uncertainty is a challenge many parents and caregivers struggle with as it feels vague in a time when all you really want is answers and clarity.
Watch and wait basically means, ‘Let’s wait and see how things develop’ with the child, their symptoms and any associated medical concerns. For some this increases anxiety and questions of ‘What am I waiting for?’ – for others it’s a relief that there’s nothing so concerning that it needs immediate treatment or interventions.
Our advice to anyone in this situation is to ask your medical professional if there’s anything specific that you should be watching out for (the list above should help) and ensure you know who to contact if there any changes in your child’s symptoms or condition that cause you concern – that could be your GP, your child’s paediatrician or one of the various specialists that your child may be referred to.
What should I tell my child about their diagnosis?
Be honest with your child from the start and be open about the condition with them and those around them. Childhood Tumour Trust have a booklet you can read online, featuring their mascot ‘Patches’, to help explain to children their diagnosis – you can order a printed copy here. There is also a video to watch for other people such as family and friends.
What happens after Diagnosis?
Now that your child has been diagnosed, you may be wondering what happens next. You can read online or order a booklet based on this website to help manage your child’s care. You can download our insert for the Red RCPCH Child Development Book – or use it on its own if your child doesn’t have one. It helps you and your healthcare provider track key health concerns, along with the NF1 Review Checklist for children and adults. Your child might not be prescribed any treatment in the first instance. Instead, you may be asked to keep a close eye on your child’s health and behaviour, to monitor for any changes. Such changes can include:
-
New lumps or bumps, or changes to existing ones
-
Headaches
-
Alterations to speech
-
Changes in their ability to move around
-
Difficulties with social interactions
-
Sensitivity to light, noise, touch, tastes, or smells
-
Changes in eyesight
Quite often families of children with NF1 will hear the phrase, ‘watch and wait’ or something similar. What this means and how to deal with this period of uncertainty is a challenge many parents and caregivers struggle with as it feels vague in a time when all you really want is answers and clarity.
Watch and wait basically means, ‘Let’s wait and see how things develop’ with the child, their symptoms and any associated medical concerns. For some this increases anxiety and questions of ‘What am I waiting for?’ – for others it’s a relief that there’s nothing so concerning that it needs immediate treatment or interventions.
Our advice to anyone in this situation is to ask your medical professional if there’s anything specific that you should be watching out for (the list above should help) and ensure you know who to contact if there any changes in your child’s symptoms or condition that cause you concern – that could be your GP, your child’s paediatrician or one of the various specialists that your child may be referred to.
Will my child grow tumours?
We understand that the word ‘tumours’ can be scary, but not all tumours are harmful. There are a number of different tumours associated with NF1, of which your child may have some or none.
Subcutaneous and cutaneous neurofibromas are small bumps that appear on or under the skin, and usually appear at puberty, but can be seen in younger children. These appear in almost everyone with NF1 at some point, but can be relatively few in number.4
Plexiform Neurofibromas can be more symptomatic. They develop in around 30-50% of those with NF1. Early signs may be an unexplained lump, or a very large café-au-lait mark that becomes thickened and may have excessive hair growth.4 It is important that these are monitored by an NF1 specialist, and an appointment is made if there is any rapid increase in growth or pain. If they become symptomatic, surgery is often the first option.4
Optic pathway gliomas (OPGs) (sometimes described simply as “brain tumours”) are lumps that grow on the optic nerves. They can cause problems with vision, so it is essential to have regular check-ups with an ophthalmologist, and they usually appear up to the age of 7. These are slow growing tumours and there is often no treatment needed other than regular monitoring. If any issues arise prognosis is normally good with the appropriate treatment.4
It’s important to clarify with your healthcare professional what type of tumour your child has if any. Additionally, there are things called ‘Unidentified Bright Objects’ (UBOs) that are commonly found in the brains of individuals with NF1. These are areas that appear bright on MRI scans and are harmless. However, they are sometimes mistakenly referred to as tumours, which can cause unnecessary concern. It’s crucial to understand whether what has been identified is truly a tumour or something benign like a UBO.
Always ask your healthcare provider for clear information about the nature of any findings, so you can better understand what it means for your child’s health.
What can I do to help my child?
It’s crucial that you and your child attend all their appointments, such as eye tests, scans in hospital and check-ups with the paediatrician, which should include a blood pressure check.
It is not uncommon for children with NF1 to have sleep problems, which you should discuss this with your medical team. Options are available including prescribed medication such as melatonin.
As with all children, your child should be encouraged to eat a healthy balanced diet, which is not always easy. They might need additional supplements such as Vitamin D, which your healthcare practitioner may want to discuss with you after a blood test. Additionally, some children with NF1 may benefit from L-Carnitine, which can help with muscle tone—please discuss this with your healthcare provider.
You might want to find out if there are any clinical research studies currently enrolling that may be suitable for you and your child. Search on clinicaltrials.gov to see what’s out there. Always ask your doctor if you’re unsure about anything.
You may also find your child needs more help at school, ensure your child’s educational placement is informed, including the school nurse, of the possible learning and health implications of NF1.
Many children with NF1 may need an MRI at some point during their childhood, though not all will. For younger children, MRIs are often done under general anesthetic, but as they get older, this may no longer be an option. Preparing your child for the experience can make a big difference. Our booklet, featuring our mascot Patches, tells the story of this first MRI in a child-friendly way to help ease any worries . Additionally, we offer a downloadable recording of an MRI scanner. While the sounds may not match exactly, it can help familiarise your child with what to expect.
Who could be in my child’s healthcare team?
Paediatrician
Paediatricians treat children, so you’ll probably get to know this team member quite well.
Ideally, your child’s paediatrician should have experience in NF1 and should know when to bring in other experts to give your child the best possible care.
Ophthalmologist /Optometrist
Ophthalmologists specialise in the examination and treatment of the eyes. They should perform check-ups annually until the age of 8.
After that, there should be annual checks by an optometrist or an optician who can test for any changes in your child’s vision.
School Nurse
The school nurse is to ensure that your child gets the right support around their medical needs in school.
Physiotherapist / Occupational Therapist
They will help with fine and gross motor skills, mobility and function and emotional regulation.
What tests are used to monitor a child?
| What is the test? | What’s it like? | What’s it for? |
|---|---|---|
| Magnetic Resonance Imaging (MRI) | The MRI machine is tunnel shaped. It’s designed for a person to lie inside it while being scanned. It can take a while, and the person being scanned needs to keep still. The machine makes quite a lot of noise, too, so your child may be given some medication to keep them calm, or even a general anaesthetic if they are very young so they keep still during the scan. Some hospitals allow a film or music be played to help your child. Childhood Tumour Trust have a recording of an MRI which is useful to play when reading a story in the weeks leading up to a scan so they can get used to the noise. The MRI scanner uses magnetic waves to create a ‘map’ of the inside of your child’s body. It doesn’t use any radiation so shouldn’t cause any harm. |
MRI is useful for diagnostic and monitoring purposes because it can find small changes in your child’s condition. |
| Ultrasound Scans | Ultrasound is commonly used for monitoring pregnancies. It uses sound waves to define the edges of structures inside the body. Special gel is rubbed over the part of the body being scanned to conduct the sound waves more easily, then the ultrasound technician will move the probe around over the skin to build a map of the inside of your child’s body. Ultrasound doesn’t use any radiation, and there are no known risks from the procedure. |
Ultrasound can be used as an alternative non-invasive scan. |
| Ophthalmology | There are a lot of different tests that an ophthalmologist will perform to check your child’s eyesight. Basic Vision Tests: These are the type of tests that you might have at a normal check-up at the opticians. These check for blind spots, blurry vision, colour vision, how the pupils react to light, etc. After these tests, your child’s sight might be quite blurry for a bit and they need to wait until it goes back to normal before, for example, returning to school. |
If your ophthalmologist detects signs of vision loss, they should recommend an MRI of your child’s head (see above for more about MRIs). |
| Annual Paediatric Visit | As per the assessments to diagnose NF1, your child will have an annual check-up with a paediatrician to review their symptoms. | This is to monitor your child, to see what – if anything – has changed over the course of 12 months. The paediatrician can refer your child to a specialist or prescribe treatment, depending on whether they notice any changes that need addressing. |
Your healthcare team should avoid X-rays or computer tomography (CT) scans wherever possible, as these involve radiation. Neurofibromas are particularly sensitive to radiation and exposure could trigger more growth. However, there are times when they are necessary and should be used.
What can I do to help my child?
It’s crucial that you and your child attend all their appointments, such as eye tests, scans in hospital and check-ups with the paediatrician, which should include a blood pressure check.
It is not uncommon for children with NF1 to have sleep problems, which you should discuss this with your medical team. Options are available including prescribed medication such as melatonin.
As with all children, your child should be encouraged to eat a healthy balanced diet, which is not always easy. They might need additional supplements such as Vitamin D, which your healthcare practitioner may want to discuss with you after a blood test. Additionally, some children with NF1 may benefit from L-Carnitine, which can help with muscle tone—please discuss this with your healthcare provider.
You might want to find out if there are any clinical research studies currently enrolling that may be suitable for you and your child. Search on clinicaltrials.gov to see what’s out there. Always ask your doctor if you’re unsure about anything.
You may also find your child needs more help at school, ensure your child’s educational placement is informed, including the school nurse, of the possible learning and health implications of NF1.
Many children with NF1 may need an MRI at some point during their childhood, though not all will. For younger children, MRIs are often done under general anesthetic, but as they get older, this may no longer be an option. Preparing your child for the experience can make a big difference. Our booklet, featuring our mascot Patches, tells the story of this first MRI in a child-friendly way to help ease any worries . Additionally, we offer a downloadable recording of an MRI scanner. While the sounds may not match exactly, it can help familiarise your child with what to expect.
Who could be in my child’s healthcare team?
Paediatrician
Paediatricians treat children, so you’ll probably get to know this team member quite well.
Ideally, your child’s paediatrician should have experience in NF1 and should know when to bring in other experts to give your child the best possible care.
Ophthalmologist /Optometrist
Ophthalmologists specialise in the examination and treatment of the eyes. They should perform check-ups annually until the age of 8.
After that, there should be annual checks by an optometrist or an optician who can test for any changes in your child’s vision.
School Nurse
Physiotherapist / Occupational Therapist
What tests are used to monitor a child?
| What is the test? | What’s it like? | What’s it for? |
|---|---|---|
| Magnetic Resonance Imaging (MRI) | The MRI machine is tunnel shaped. It’s designed for a person to lie inside it while being scanned. It can take a while, and the person being scanned needs to keep still. The machine makes quite a lot of noise, too, so your child may be given some medication to keep them calm, or even a general anaesthetic if they are very young so they keep still during the scan. Some hospitals allow a film or music be played to help your child. Childhood Tumour Trust have a recording of an MRI which is useful to play when reading a story in the weeks leading up to a scan so they can get used to the noise. The MRI scanner uses magnetic waves to create a ‘map’ of the inside of your child’s body. It doesn’t use any radiation so shouldn’t cause any harm. |
MRI is useful for diagnostic and monitoring purposes because it can find small changes in your child’s condition. |
| Ultrasound Scans | Ultrasound is commonly used for monitoring pregnancies. It uses sound waves to define the edges of structures inside the body. Special gel is rubbed over the part of the body being scanned to conduct the sound waves more easily, then the ultrasound technician will move the probe around over the skin to build a map of the inside of your child’s body. Ultrasound doesn’t use any radiation, and there are no known risks from the procedure. |
Ultrasound can be used as an alternative non-invasive scan. |
| Ophthalmology | There are a lot of different tests that an ophthalmologist will perform to check your child’s eyesight. Basic Vision Tests: These are the type of tests that you might have at a normal check-up at the opticians. These check for blind spots, blurry vision, colour vision, how the pupils react to light, etc. After these tests, your child’s sight might be quite blurry for a bit and they need to wait until it goes back to normal before, for example, returning to school. |
If your ophthalmologist detects signs of vision loss, they should recommend an MRI of your child’s head (see above for more about MRIs). |
| Annual Paediatric Visit | As per the assessments to diagnose NF1, your child will have an annual check-up with a paediatrician to review their symptoms. | This is to monitor your child, to see what – if anything – has changed over the course of 12 months. The paediatrician can refer your child to a specialist or prescribe treatment, depending on whether they notice any changes that need addressing. |
Your healthcare team should avoid X-rays or computer tomography (CT) scans wherever possible, as these involve radiation. Neurofibromas are particularly sensitive to radiation and exposure could trigger more growth. However, there are times when they are necessary and should be used.
Where can I find support?
Childhood Tumour Trust Facebook Group
Tumour Support Scotland
Nerve Tumours UK
NF Patients United
Will my child need help at school?
The majority of children with NF1 will have an average or above average IQ; they often just need different teaching methods to help them fully engage with learning. Common associated conditions include:
-
Autism and ADHD traits
-
General learning difficulties
-
Specific learning difficulties such as dyslexia or dyscalculia
-
Sensory processing difficulties
-
Speech / language / communication difficulties
-
Memory difficulties
-
Difficulties with processing
Some children and young people will need additional help in school and will be placed on the SEN register, meaning the school will have an individual learning plan for them to ensure they get the help they require. If additional support is needed, the school or parents can apply for an Education, Health and Care Plan (EHCP) to ensure all their needs are identified and met.
What an EHCP can do to help…
Frequently asked questions
1. Is NF1 life limiting?
NF1 is not life limiting for most children but some of its rare complications can cause serious – possibly life-threatening – health problems, which is why we emphasise the importance of getting every symptom checked.
2. What are the serious signs I should look for?
3. Will my child develop tumours?
4. Will they be in pain?
5. What do I tell my child about the diagnosis?
6. Who can I talk to?
7. Will my child need help in school?
8. Can my child still live independently when they grow up?
References
- Tamura R. Current Understanding of Neurofibromatosis Type 1, 2, and Schwannomatosis. Int J Mol Sci. 2021;22(11).
- Cancer Research UK. Genes, DNA and cancer. Available at: www.cancerresearchuk.org Last accessed March 2022.
- University of Alabama at Birmingham: School of Medicine Neurofibromatosis Program. Inheritance and Genetics of Neurofibromatosis Type 1 (NF1).
Available at: www.uab.edu Last accessed March 2022. - Ferner RE, Huson SM, Thomas N, et al. Guidelines for the diagnosis and management of individuals with neurofibromatosis 1. J Med Genet. 2007;44(2):81-8.
Our stories of living with NF1

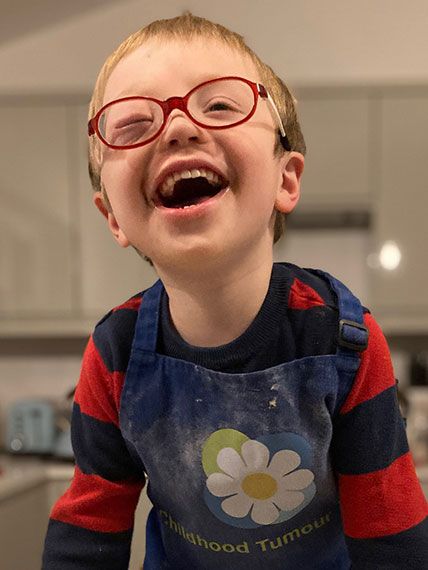
Austin
Our son Austin is 8 years old. He was diagnosed with NF1 aged 3 after we noticed many café-au-lait marks and freckling. The journey to diagnosis was a struggle, but was confirmed after genetic testing. No-one in the family carries the gene. Austin is hypermobile, has speech and language difficulties and some mild learning differences. He is currently classed as ‘mild’. Austin has a diagnosis of autism and thrives in education. He is an elected school ambassador and also a keen member of the chess club.

Nicole
When my daughter Nicole was born, her café-au-lait marks were dismissed as birth marks. When she was 3 it was suggested that she had NF1 due to the café-au-lait patches and delayed speech. Nicole was the first in the family to be diagnosed with NF1 and it has been a learning curve. She has a large plexiform wrapped around her sciatic nerve, scoliosis and ASD. Despite most of her childhood going in and out of hospital for scans, surgery and appointments, and struggling through school, she is finishing her degree in Design Engineering living independently and travelling the world. She is proud of who she is and wants to advocate for others. In her words, she can do almost anything anyone else can – just sometimes a bit differently. Learning to live with NF1 will take time, and nobody can predict the pathway ahead but the important thing as a parent/carer is to be aware of changes in the condition, who to see and when, to recognise that NF1 is part of your child and everything else will follow.

Dan

Clare